|
Senior Member
Join Date: Feb 2008
Location: South East Wisconsin
Posts: 3,431
|
Brain mets
Extensive 9/27/2010 overview of brain/CNS mets treatments from Breast Cancer Watch:
http://bcwatchdigest-brain.evidencewatch.com/
J Neurooncol. 2007 Mar;82(1):91-3. Epub 2006 Sep 26.
A lipoxygenase inhibitor in breast cancer brain metastases.(Boswellia serrata)
PDF(3pgs): http://www.springerlink.com/content/...2/fulltext.pdf
Flavin DF.
Foundation for Collaborative Medicine and Research, Greenwich, CT 06831, USA. Dana_FK@hotmail.com
The complication of multiple brain metastases in breast cancer patients is a life threatening condition with limited success following standard therapies. The arachidonate lipoxygenase pathway appears to play a role in brain tumor growth as well as inhibition of apoptosis in in-vitro studies. The down regulation of these arachidonate lipoxygenase growth stimulating products therefore appeared to be a worthwhile consideration for testing in brain metastases not responding to standard therapy.
Boswellia serrata, a lipoxygenase inhibitor was applied for this inhibition. Multiple brain metastases were successfully reversed using this method in a breast cancer patient who had not shown improvement after standard therapy. The results suggest a potential new area of therapy for breast cancer patients with brain metastases that may be useful as an adjuvant to our standard therapy.
PMID: 17001517 [PubMed - indexed for MEDLINE]
Quote:
The patient was started on capecitabine and given radiation therapy of 44 Gy with no improvement seen for the first 2 weeks. The severity and inoperability of
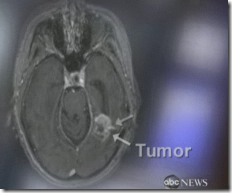
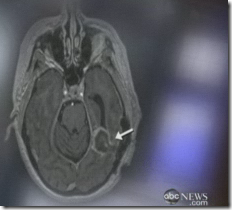
her condition made using an additional therapy a consideration. An oxidoreductase [plant lipoxygenases (LOX)] inhibitor was applied (Boswellia serrata) which has no known major side effects. The enzyme, LOX, arachidonate: oxygen oxidoreductase (form mammalian LOX) is thought to be responsible for edema in primary brain tumors and present ongoing studies on LOX inhibitors in Germany indicate an overall improvement in response to radiation therapy as well as a decrease in some primary brain tumors seen even without radiation. Although it was not known if LOX inhibitors would be helpful in breast cancer brain metastases it was worth considering in this case since she had not only several large tumors but also additional extremely small tumors scattered throughout the brain. She was immediately placed on a LOX inhibitor. Following 10 weeks of therapy, the patient was scheduled for a new CT since her CEA and Ca 15–3 tumor markers had increased. The CT results showed a complete disappearance of all signs of metastases in her brain (Fig. 2a, b).
The patient has been maintained on the LOX inhibitor,
Boswellia serrata, 3 · 800 mg/day
with no new signs of cerebral involvement of her breast cancer for over 4 years, however, there have recently been skeletal metastases which most likely indicates LOX has a limited skeletal tissue involvement in cancer.
|
Boswellia serrata
http://www.cancersalves.com/botanica...boswellia.html
Prof. Thomas Simmet has researched Boswellia serrata on astrocytomes, a tumor noted for its propensity to metastasize. Prof. Simmet's background is in pharmacology, and he suggests that the boswellic acids reduce inflammation. I was familiar with this research because boswellia is used extensively in Ayurveda to reduce the symptoms of arthritis. Prof. Simmet proposes that boswellia inhibits the production of an enzyme that causes the leukotriene production associated with inflammation. In laboratory tests, Prof. Simmet observed that the more malignant the tumor, the more leukotrienes it produces. This seems to perpetuate a cycle of almost unstoppable growth. Working with a neurosurgeon, Michael Winking, 25 patients were administered a dry extract of boswellia for one week. The tumors were then surgically removed. About half the patients had such significant regressions that the tumors had all but disappeared. They used a dosage of 800 mg. three times a day. | CT before Boswellia | | CT after Boswellia [10 weeks] | CT images compliments of Dr. Dana Flavin-Koenig
Foundation for Collaborative Medicine and Research
|
| At the university hospitals of Bochum and Giessen, patients with gliome tumors were administered somewhat higher dosages of Boswellia serrata, 3600 mg. per day. Within only a few days, many symptoms associated with brain tumors, such as headaches and lameness, were greatly lessened. While much of this effect might be more related to the reduction in edema than to the regression of the tumor, swelling and the resultant pressures are serious side effects of malignancy that impact the quality of life. The reports of these trials are preliminary and researchers are unwilling to speculate as to the long-term results and whether or not tumor growth is arrested.
Planta Med. 2000 Mar;66(2):110-3.
Concentration-dependent potentiating and inhibitory effects of Boswellia extracts on 5-lipoxygenase product formation in stimulated PMNL.
Safayhi H, Boden SE, Schweizer S, Ammon HP.
Department of Pharmacology, University of Tuebingen, Germany. hasan.safayhi@uni-tuebingen.de
Preparations from the gum of Boswellia spec. have been used in the traditional medicine for the treatment of inflammatory diseases. Extracts from B. serrata gum were shown to inhibit leukotriene biosynthesis by impairing the 5-lipoxygenase (5-LO) activity. In order to identify the minimal effective concentrations of extracts in vitro we studied the effects of ethanolic extracts from commercially available resins from two regions (B. serrata gum from India and Olibanum in granis from Arabia) on the 5-LO product formation from endogenous substrate in calcium and ionophore stimulated neutrophils in a defined concentration range. Both extracts inhibited 5-LO product formation in vitro in concentrations greater than 10 to 15 micrograms/ml as reported previously for an ethanolic B. serrata extract. In contrast, lower concentrations of extracts (1 to 10 micrograms/ml) even potentiated 5-LO product formation, especially the biosynthesis of 5(S)-HETE. The in vitro data underline the major importance of drug standardization when Boswellia resin containing preparations are used for the treatment of diseases.
http://www.treatingglioblastoma.com/...llic_acids.htm
From a wide variety of studies, boswellic acids have been shown to:
- Inhibit leukotriene biosynthesis
- Inhibit 5-lipoxygenase
- Inhibit topoisomerase I
- Inhibit topoisomerase IIalpha
- Induce apoptosis in glioma cells
- Inhibit NF-kappaB
- Reduce diarrhea
Further research into the constituent components of boswellia indicate that it is also directly cytotoxic to brain tumor cancer cells. Boswellia extracts have been shown to be both cytotoxic to glioma cells and anti-proliferative in a dose-dependent manner during studies with rats 10.
J Neurooncol. 2009 Jan;91(1):47-50. Epub 2008 Aug 19.
Long-lasting successful cerebral response with sorafenib in advanced renal cell carcinoma.
Valcamonico F, Ferrari V, Amoroso V, Rangoni G, Simoncini E, Marpicati P, Vassalli L, Grisanti S, Marini G.
Department of Medical Oncology, Spedali Civili di Brescia, Brescia, Italy. franzval@yahoo.it
We report the case of a 75-year old woman who received sorafenib (Nexavar), Bayer Pharmaceuticals Corporation, West Haven, CT) for a CNS relapse of clear cell renal cell carcinoma. After four months of sorafenib treatment, a brain magnetic resonance imaging showed 95%-volumetric regression of cerebral metastasis. To the best of our knowledge, this is the first almost complete resolution of brain metastases in renal cell carcinoma treated with sorafenib that has been described.
PMID: 18712279 [PubMed - indexed for MEDLINE]
PMID: 10763581 [PubMed - indexed for MEDLINE]
Noscapine Crosses the Blood-Brain Barrier and Inhibits Glioblastoma Growth
Full Text: http://clincancerres.aacrjournals.or...0/15/5187.full
Abstract
The opium alkaloid noscapine is a commonly used antitussive agent available in Europe, Asia, and South America. Although the mechanism by which it suppresses coughing is currently unknown, it is presumed to involve the central nervous system. In addition to its antitussive action, noscapine also binds to tubulin and alters microtubule dynamics in vitro and in vivo. In this study, we show that noscapine inhibits the proliferation of rat C6 glioma cells in vitro (IC 50 = 100 μm) and effectively crosses the blood-brain barrier at rates similar to the ones found for agents such as morphine and [Met]enkephalin that have potent central nervous system activity ( P ≤ 0.05). Daily oral noscapine treatment (300 mg/kg) administered to immunodeficient mice having stereotactically implanted rat C6 glioblasoma into the striatum revealed a significant reduction of tumor volume ( P ≤ 0.05). This was achieved with no identifiable toxicity to the duodenum, spleen, liver, or hematopoietic cells as determined by pathological microscopic examination of these tissues and flow cytometry. Furthermore, noscapine treatment resulted in little evidence of toxicity to dorsal root ganglia cultures as measured by inhibition of neurite outgrowth and yielded no evidence of peripheral neuropathy in animals. However, evidence of vasodilation was observed in noscapine-treated brain tissue. These unique properties of noscapine, including its ability to cross the blood-brain barrier, interfere with microtubule dynamics, arrest tumor cell division, reduce tumor growth, and minimally affect other dividing tissues and peripheral nerves, warrant additional investigation of its therapeutic potential.
Artemisinin is thought to penetrate the CNS and may work: LINK to thread
Brain Cancer Treatment Kills Tumors by 'Cooking' with Laser– Cleveland Clinic
Posted Feb 24 2009 10:44pm
This a brand new technique and is not FDA approved yet, but they are hoping by the end of the year to have approval on this process. 
There is a video at the link that explains more. From the pictures below it certainly looks at though it has done something for the patient who had a brain tumor that grew back. The patient had to be kept unconscious for 12 hours for the procedure to take place. I am guessing this could also work on other areas of the body too with tumors.
Body temperature is maintained as the patient is inside an MRI for the entire procedure. This procedure is offering hope to those who have had what has been considered inoperable surgery for their brain tumors. BD Ruth Perko is one of at least 97,000 Americans diagnosed with a malignant brain tumor each year, according to the National Cancer Institute, and nothing can prepare her for the experimental treatment she's about to receive.
With the probe now inside Perko's brain tumor, doctors fire the laser. Each burst lasts anywhere from 30 seconds to a few minutes and generates up to 160 degrees (Fahrenheit) of heat, enough to restrict blood flow to the area and kill the cancer cells. Doctors carefully monitor the temperature by keeping Perko in an MRI machine throughout the procedure.
"We can monitor the temperature rise in the tumor, second by second, while we're scanning the patient," said Dr. Stephen Jones, a neuro radiologist at the Cleveland Clinic. "Better than that," he said, "we can see the predictive margins of response where we are killing the tumor... where the cancer cells are dying."
This is the before picture.
This is the after picture.
Cancer. 2009 Nov 20. [Epub ahead of print]
Disruption of the blood brain barrier by brain metastases of triple-negative and basal-type breast cancer but not HER2/neu-positive breast cancer.
Yonemori K, Tsuta K, Ono M, Shimizu C, Hirakawa A, Hasegawa T, Hatanaka Y, Narita Y, Shibui S, Fujiwara Y.
Breast and Medical Oncology Division, National Cancer Center Hospital, Tokyo, Japan.
BACKGROUND:: Generally, the blood-brain barrier (BBB) of brain metastasis was thought to be disrupted. METHODS:: We retrospectively performed immunohistochemical staining for glucose transporter 1 (GLUT1) and breast cancer resistance protein (BCRP) to evaluate the status of the BBB in resected brain metastases. Associations between expression of GLUT1 and/or BCRP and the immunohistochemical profiles of breast cancers, such as the statuses of hormone receptors, human epidermal growth factor receptor 2 (HER2/neu), and a basal-type marker (cytokeratin 5/6, HER1), were also analyzed. RESULTS:: The study included 29 breast cancer patients with brain metastasis who had undergone brain tumor resections. Among the 29 patients, there was no expression of GLUT1 and BCRP in the intratumor microvessels of 9 (32%) and 11 (38%) patients, respectively. There was no expression of both GLUT1 and BCRP in 8 patients (28%). The expression of GLUT1 was significantly associated with that of BCRP (P < .001). A positive correlation was observed between the expression of GLUT1 and/or BCRP and brain metastases of HER2/neu-positive breast cancer (P = .012), while a negative correlation was observed between the expression of GLUT1 and/or BCRP and brain metastases of triple negative or basal-type breast cancer (P = .014 and P = .003 for triple negative and basal-type, respectively). CONCLUSIONS:: Brain metastases of triple negative or basal-type breast cancers may often disrupt the BBB, whereas brain metastases of HER2/neu-positive breast cancer tend to preserve the BBB. Cancer 2010. (c) 2009 American Cancer Society.
PMID: 19937674
Xeloda/5fu for brain mets?
Behav Brain Res.. [Epub ahead of print]
Fluoxetine improves the memory deficits caused by the chemotherapy agent 5-fluorouracil.
Elbeltagy M, Mustafa S, Umka J, Lyons L, Salman A, Chur-Yoe GT, Bhalla N, Bennett G, Wigmore PM.
Department of Anatomy, Menoufiya University, Egypt; School of Biomedical Sciences, Institute of Neuroscience, University of Nottingham, Queen's Medical Centre, Nottingham NG7 2UH, UK.
Cancer patients who have been treated with systemic adjuvant chemotherapy have described experiencing deteriorations in cognition. A widely used chemotherapeutic agent, 5-fluorouracil (5-FU), readily crosses the blood-brain barrier and so could have a direct effect on brain function. In particular this anti mitotic drug could reduce cell proliferation in the neurogenic regions of the adult brain. In contrast reports indicate that hippocampal dependent neurogenesis and cognition are enhanced by the SSRI antidepressant Fluoxetine. In this investigation the behavioural effects of chronic (two week) treatment with 5-FU and (three weeks) with Fluoxetine either separately or in combination with 5-FU were tested on adult Lister hooded rats. Behavioural effects were tested using a context dependent conditioned emotional response test (CER) which showed that animals treated with 5-FU had a significant reduction in freezing time compared to controls. A separate group of animals was tested using a hippocampal dependent spatial working memory test, the object location recognition test (OLR). Animals treated only with 5-FU showed significant deficits in their ability to carry out the OLR task but co administration of Fluoxetine improved their performance. 5-FU chemotherapy caused a significant reduction in the number of proliferating cells in the sub granular zone of the dentate gyrus compared to controls. This reduction was eliminated when Fluoxetine was co administered with 5-FU. Fluoxetine on its own had no effect on proliferating cell number or behaviour. These findings suggest that 5-FU can negatively affect both cell proliferation and hippocampal dependent working memory and that these deficits can be reversed by the simultaneous administration of the antidepressant Fluoxetine.
PMID: 19914299 [PubMed - as supplied by publisher]
Concurrent capecitabine and whole-brain radiotherapy for treatment of brain metastases in breast cancer patients
Cyrus Chargari2, Youlia M. Kirova2  , Véronique Diéras2, Pablo Castro Pena2, Francois Campana2, Paul H. Cottu2, JeanYves Pierga2, Alain Fourquet2 and Institut Curie Breast Cancer Study Group1 , Véronique Diéras2, Pablo Castro Pena2, Francois Campana2, Paul H. Cottu2, JeanYves Pierga2, Alain Fourquet2 and Institut Curie Breast Cancer Study Group1 | (1) | Institut Curie, Paris, France | | (2) | Department of Radiation Oncology, Department of Medical Oncology, Institut Curie, 26, Rue d’Ulm, 75005 Paris, France | Received: 23 September 2008 Accepted: 30 December 2008 Published online: 25 January 2009
Abstract Preclinical data have demonstrated that ionizing radiation acts synergistically with capecitabine. This report retrospectively assessed the use of capecitabine concurrently with whole-brain radiotherapy (WBRT) in patients with brain metastases from breast cancer. From January 2003 to March 2005, five breast cancer patients with brain metastases were referred for WBRT with concurrent capecitabine. Median age was 44 years (range: 38–53). The median dose of capecitabine was 1,000 mg/m2 twice daily for 14 days (day1–14). Treatment cycles were repeated every 21 days, concurrently with WBRT (30 Gy, 3 Gy per fraction, 5 days per week). Median survival after starting WBRT plus capecitabine was 6.5 months (range 1–34 months). One patient achieved a complete response. Two patients achieved partial response, including one with local control lasting until most recent follow-up. One patient had stable disease. The remaining patient was not assessable for response because of early death. Most commonly reported adverse events were nausea (n = 2) and headache (n = 2), always grade 1. Other toxicities were grade 3 hand/foot syndrome (n = 1), moderate anemia requiring transfusion and dose reduction of capecitabine (n = 1), and grade 1 mucositis (n = 1). Although promising, these preliminary data warrant further assessment of capecitabine-based chemoradiation in brain metastases from breast cancer and need to be further validated in the setting of a clinical trial.
http://www.ohsu.edu/xd/education/sch...le-display.cfm Edward Neuwelt, M.D.
Title: Professor
Email: neuwelte@ohsu.edu
Primary Affiliation
Blood Brain Barrier and Neuro-Oncology Program Program Affiliations- Neuroscience Graduate Program
- Neurology
Background Edward A. Neuwelt, M.D. is a Professor in the Departments of Neurology and Neurosurgery at Oregon Health & Science University and the Portland Veterans Affairs Medical Center in Portland, Oregon. He divides his time between clinical work, primarily in the area of neuro-oncology including both operative neurosurgery and chemotherapy, and directing his research laboratory.
Program History
In the early 1980s, Edward A. Neuwelt, M.D., an OHSU neurosurgeon, pioneered a unique method of outwitting the brain's protective blood-brain barrier. By temporarily opening this barrier, chemotherapy, antibodies and other potential new therapeutics can pass into the brain and reach the tumor.
Since then, Dr. Neuwelt has devoted his neuro-oncology practice to researching and refining this treatment for patients with brain tumors. A recent development is the use of chemoprotective agents which may provide bone marrow and hearing protection for patients undergoing platinum-based chemotherapy with BBBD.
Faculty Appointments:
In Texas, Dr. Neuwelt was Assistant Professor in both Surgery and Biochemistry at the University of Texas Southwestern Medical School. He was also Chief of the Neurosurgery Service at the Dallas Veterans Administration Hospital in Dallas, Texas from 1978 – 1981. Dr. Neuwelt moved his laboratory to Portland Oregon in 1981 where he joined the faculty at the Oregon Health & Science University, both in the Department of Neurology and Biochemistry and Molecular Biology. He was Chief of the Neurosurgery Service at the Veterans Affairs Medical Center in Portland, Oregon 1981 – 1989, and he maintains an affiliation with the Portland VA Neurosurgery Service. Currently Dr. Neuwelt is a Professor in the departments of Neurology and Neurological Surgery. He is a member of the Neuroscience Graduate Program and the Biochemistry and Molecular Biology Graduate Program at OHSU, and also regularly teaches the neurology and neurosurgery house staff on topics related to brain tumors.
Activities and Organizations:
Dr. Neuwelt is the principal investigator of three NIH R01 grants, one VA Merit Review grant, and a DOD Center of Excellence award. (see Preclinical Research) He has been a regular member of the VA Merit Review Study Section on Neurobiology, and an NIH Study Section (NSP-A) that reviews program project and center grants. Dr. Neuwelt is a regular reviewer of neuroscience-related journals, including Neurosurgery, for which he was a member of the editorial board. He initiated and is director of Think First Oregon, a brain and spinal cord injury prevention program. He has eight approved patents, five of which have been licensed to Adherex, Inc. to investigate thiol agent chemoprotection. In collaboration with Dr. James Rosenbaum and Dr. Richard Rosenbaum, Dr. Neuwelt set up and directs a science class for high school students that introduces young people to laboratory research. With regard to the BBB Program, Dr. Neuwelt has overseen the expansion of the program to eight institutions across the US and internationally including Canada and Israel, as well as the annual Blood-Brain Barrier (BBB) Consortium meeting funded by an R13 grant.
Research Interests
The OHSU Blood-Brain Barrier and Neuro-Oncology Program conducts innovative patient-oriented research in all aspects of imaging and therapy of brain tumors. Dr. Neuwelt’s research interests have centered around the blood-brain barrier (BBB) and brain tumor therapy. In his initial VA Merit Review grant in 1978, Dr. Neuwelt predicted that manipulation of the BBB with transient osmotic shrinkage had the potential for a therapeutic role in brain tumor therapy. This hypothesis has been verified (Kraemer 2001), and the BBB disruption technique is now central to the preclinical and clinical research studies in the Neuwelt laboratory. Overall, Dr. Neuwelt’s research interests have centered around improving brain tumor therapy, reducing chemotherapy side effects, and improving brain tumor imaging. Dr. Neuwelt currently has a VA Merit review grant, three NIH research grants, an R13 NIH meeting grant, and is a member of a DOD breast cancer Center of Excellence.
Cancers in the brain are difficult to treat because of neurotoxicity, tumor resistance, and minimal delivery of potential therapies across the blood-brain barrier. We do basic science and preclinical studies of new approaches to delivery, treatment, and imaging in primary and metastatic brain tumor models.
Selected Publications
Dr. Neuwelt has written or edited several books and book chapters, and has over 200 peer reviewed scientific publications. Please refer to his listing here
Education
Dr. Neuwelt attended Northwestern University in Chicago, Illinois from 1965 – 1968 and then received his M.D., magna cum laude, from the University of Colorado School of Medicine in Denver, Colorado in 1972. For his postgraduate Training, Dr. Neuwelt did a surgical internship at the University of Texas Southwestern Medical School in Dallas, Texas, 1972 – 1973, followed by a Neurosurgical Residency at the same institution from 1973 – 1978. During this time, Dr. Neuwelt also completed two neuro-oncology and neurosurgery research fellowships, first at the National Cancer Institute, National Institutes of Health (NIH) (1974 – 1976) and then Queen Square Hospital in London, England (1976). While at the NIH, Dr. Neuwelt also completed his military duty as a Clinical Associate (Lt. Commander) in the United States Public Health Service, Neurosurgery and Enzymology Sections in Baltimore, Maryland (July, 1974 - July, 1976). Dr. Neuwelt is certified by the American Board of Neurological Surgery and is a fully trained neuro-oncologist.
Links
Neuro-Oncology Blood-Brain Barrier Program
Links
German researchers detail how metastatic cancer takes root in the brain
By Greg Freiherr | January 11, 2010
LINK
As many as one in four cancer patients develop metastatic cancers of the brain. Existing therapies seldom do more than slow the disease. Adding to the urgency to find a way to prevent brain metastasis is the increasing number of such cases.
"Improvements in the treatment of malignancy have enhanced survival time," said Dr. Frank Winkler, who leads the Neurooncology Research Group at the Ludwig-Maximilians-Universität (LMU) Neurological Clinic in Munich. "But this also means that more patients are at risk of developing brain metastases."
In the hope of finding ways to stop this process, Winkler and colleagues at LMU and neighboring Max Planck Institute for Neurobiology have defined, in animals, the steps that lead some tumor cells to metastasize. Reporting days before Christmas in the online version of Nature Medicine, Winkler and colleagues detailed the process of brain metastasis. To do so they used two-photon microscopy to look deeply into animal tissues and visualize at high resolution structures that lay hundreds of micrometers below the surface of the living brain.
The metastatic process begins, they found, when circulating tumor cells are trapped in a network of blood vessels. The cells then pass through tiny gaps between cells in the vessel wall, escaping into the surrounding brain tissue, yet sticking to the outer surface of the vessel. Here is where the process begins in earnest, as between four and fifty cells form micrometastases that ultimately fuse, triggering the growth of new blood vessels to feed the mass.
Interrupting any one of the steps will stop metastatic cancer in its tracks, according to Winkler. His team is now looking for ways to do exactly that. One may already be at hand. In their animal research, the team detailed how the anticancer drug Avastin can suppress the emergence of metastases by blocking the formation of new blood vessels. In the absence of such angiogenesis, even cells that had attached to the outer vessel wall and proliferated strongly at first eventually died, he says.
"We now want to test other types of cancer drugs for their effects on the single steps of metastasis formation," Winkler said. "It may be possible to discover new substances that allow us to treat existing metastases effectively, or even prevent them from developing at all."
Nat Med. 2010 Jan;16(1):116-22. Epub 2009 Dec 20.
Real-time imaging reveals the single steps of brain metastasis formation.
Kienast Y, von Baumgarten L, Fuhrmann M, Klinkert WE, Goldbrunner R, Herms J, Winkler F.
Department of Neurology, Ludwig-Maximilians University, Munich, Germany.
Brain metastasis frequently occurs in individuals with cancer and is often fatal. We used multiphoton laser scanning microscopy to image the single steps of metastasis formation in real time. Thus, it was possible to track the fate of individual metastasizing cancer cells in vivo in relation to blood vessels deep in the mouse brain over minutes to months. The essential steps in this model were arrest at vascular branch points, early extravasation, persistent close contacts to microvessels and perivascular growth by vessel cooption (melanoma) or early angiogenesis (lung cancer). Inefficient steps differed between the tumor types. Long-term dormancy was only observed for single perivascular cancer cells, some of which moved continuously. Vascular endothelial growth factor-A (VEGF-A) inhibition induced long-term dormancy of lung cancer micrometastases by preventing angiogenic growth to macrometastases. The ability to image the establishment of brain metastases in vivo provides new insights into their evolution and response to therapies.
PMID: 20023634 [PubMed - indexed for MEDLINE]
Strahlenther Onkol. 2010 Feb;186(2):63-69. Epub 2010 Jan 26.
DEGRO Practical Guidelines for Palliative Radiotherapy of Breast Cancer Patients: Brain Metastases and Leptomeningeal Carcinomatosis.
Feyer P, Sautter-Bihl ML, Budach W, Dunst J, Haase W, Harms W, Sedlmayer F, Souchon R, Wenz F, Sauer R.
Klinikum Neukölln, Berlin, Germany, petra.feyer@vivantes.de.
PURPOSE: : To provide recommendations for palliative treatment of brain metastases (BM) and leptomeningeal carcinomatosis (LC) in breast cancer patients with specific emphasis on radiooncologic aspects. METHODS: : The breast cancer expert panel of the German Society of Radiation Oncology (DEGRO) performed a comprehensive survey of the literature comprising national and international guidelines, lately published randomized trials, and relevant retrospective analyses. The search included publications between 1995-2008 (PubMed and Guidelines International Network [G-I-N]). Recommendations were devised according to the panel's interpretation of the evidence referring to the criteria of EBM. RESULTS: : Aim of any treatment of BM and LC is to alleviate symptoms and improve neurologic deficits. Close interdisciplinary cooperation facilitates rapid diagnosis and onset of therapy, tailored to the individual and clinical situation. Treatment decisions for BM should be based on the allocation to three prognostic groups defined by recursive partitioning analysis (RPA). Karnofsky Performance Score (KPS) is the strongest prognostic parameter. Together with the extent of the disease, KPS determines whether excision or radiosurgery/stereotactic radiotherapy is feasible and if exclusive or additional whole-brain radiotherapy (WBRT) is indicated. With adequate therapy, survival may be up to 3 years. For LC, treatment is mostly indicated for patients with positive cytology or in case of strongly indicative signs and symptoms. Radiotherapy (WBRT and involved-field irradiation of bulky spinal lesions) and chemotherapy (systemically or intrathecally applied methotrexate, thiotepa and cytarabine) are both effective and may prolong survival from several weeks to 4-6 months. CONCLUSION: : Radiotherapy is an effective tool for palliative treatment of BM and LC.
PMID: 20127222 [PubMed - as supplied by publisher]
|